Navigating the world of diabetes can feel like a maze, especially when it comes to medications. There are so many options, each with its own mechanism and potential side effects.
From Metformin, the commonly prescribed biguanide, to newer classes like SGLT2 inhibitors and GLP-1 receptor agonists, the landscape is constantly evolving.
I’ve seen firsthand how confusing it can be for people to understand what they’re taking and why. The increasing prevalence of personalized medicine means your doctor will try to find something uniquely suitable for you.
Finding the right drug, and understanding its possible downsides, is vital for effective management and long-term health. Let’s delve into the specifics and get clarity.
Let’s get this straight!
Decoding the Alphabet Soup: Understanding Different Diabetes Medication Classes
Navigating the world of diabetes medications can feel like learning a new language. There’s a lot of jargon, and it’s easy to get lost in the details. But understanding the different classes of drugs is crucial for effective diabetes management. Each class works in a unique way to lower blood sugar levels, and knowing the basics can empower you to have more informed conversations with your doctor. From the tried-and-true Metformin to the innovative SGLT2 inhibitors, let’s break down the key players.
1. The Metformin Story: More Than Just a First Line
Metformin is often the first medication prescribed for type 2 diabetes. But its role goes beyond just being a starting point. It primarily works by decreasing glucose production in the liver and improving your body’s sensitivity to insulin. I remember when my doctor first put me on Metformin, he explained that it’s like a key that helps insulin unlock the doors of my cells, allowing glucose to enter and be used for energy. What I’ve learned over the years is that it isn’t a perfect solution. It can cause gastrointestinal issues for some people, which can be a real hassle. However, it has a long track record of safety and effectiveness, making it a cornerstone of diabetes treatment.
2. Sulfonylureas and Glinides: The Insulin Boosters
Sulfonylureas and glinides are older classes of medications that stimulate your pancreas to release more insulin. I’ve seen them work wonders for some people, providing a significant boost in insulin production. The upside is that they can be very effective at lowering blood sugar. The downside? They come with a higher risk of hypoglycemia, or low blood sugar, especially if you skip a meal or exercise vigorously. It’s also important to be aware that over time, the pancreas may become less responsive to these medications, reducing their effectiveness. This isn’t always the case, but something to keep in mind!
SGLT2 Inhibitors: A Sweet Escape Route
SGLT2 inhibitors represent a newer approach to diabetes management. They work by preventing the kidneys from reabsorbing glucose back into the blood, instead allowing excess glucose to be excreted in the urine. This not only lowers blood sugar levels but can also lead to weight loss and blood pressure reduction. When I first heard about these drugs, I was intrigued. They offered a unique way to manage diabetes without directly affecting insulin. But it’s important to note that SGLT2 inhibitors can increase the risk of urinary tract infections and yeast infections, and they may not be suitable for everyone, especially those with kidney problems.
1. The Science Behind the SGLT2 Magic
SGLT2 inhibitors target a protein called sodium-glucose cotransporter 2 (SGLT2) in the kidneys. This protein is responsible for reabsorbing glucose back into the bloodstream. By blocking this protein, SGLT2 inhibitors allow the kidneys to eliminate excess glucose through urine, effectively lowering blood sugar levels. This mechanism of action is independent of insulin, making SGLT2 inhibitors a valuable option for people with type 2 diabetes who may have reduced insulin sensitivity or production.
2. Practical Considerations: Hydration and Hygiene
Because SGLT2 inhibitors increase glucose excretion through urine, it’s crucial to stay well-hydrated while taking these medications. Drinking plenty of water can help prevent dehydration and reduce the risk of urinary tract infections. Maintaining good personal hygiene is also essential, as SGLT2 inhibitors can increase the risk of genital yeast infections. Regular check-ups with your doctor are important to monitor kidney function and overall health while on SGLT2 inhibitors.
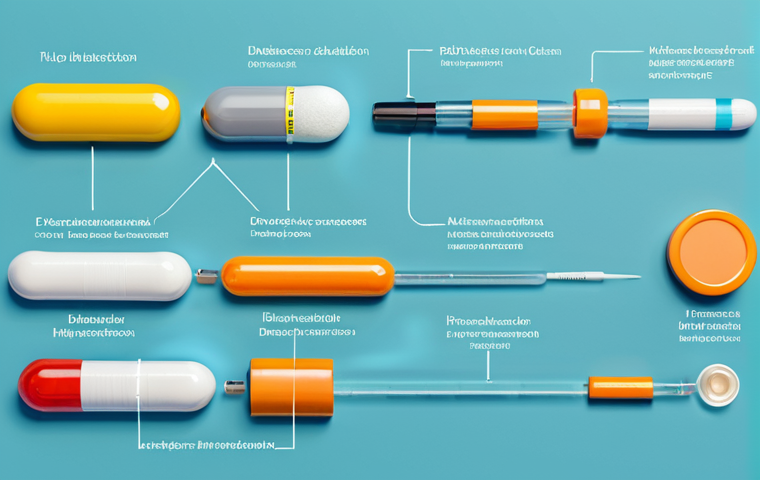
GLP-1 Receptor Agonists: More Than Just Blood Sugar Control
GLP-1 receptor agonists are injectable medications that mimic the effects of a natural hormone called glucagon-like peptide-1 (GLP-1). This hormone plays a crucial role in regulating blood sugar levels, promoting insulin release, suppressing glucagon secretion, and slowing down gastric emptying. GLP-1 receptor agonists not only lower blood sugar but can also lead to weight loss and cardiovascular benefits. I’ve heard so many people rave about the weight loss aspect, but it’s important to remember that these medications are primarily for diabetes management, and any weight loss is a bonus.
1. Appetite Control and Weight Management
One of the key benefits of GLP-1 receptor agonists is their ability to reduce appetite and promote satiety. By slowing down gastric emptying, these medications can help you feel fuller for longer, leading to reduced food intake and weight loss. This can be particularly beneficial for people with type 2 diabetes who are struggling with weight management. However, it’s important to note that the weight loss effects of GLP-1 receptor agonists can vary from person to person.
2. Potential Side Effects: Nausea and Gastrointestinal Issues
While GLP-1 receptor agonists offer numerous benefits, they can also cause side effects, particularly nausea and other gastrointestinal issues. These side effects are often mild and temporary, but they can be bothersome for some people. Starting with a low dose and gradually increasing it can help minimize these side effects. It’s also important to discuss any concerns with your doctor.
DPP-4 Inhibitors: A Gentler Approach

DPP-4 inhibitors work by preventing the breakdown of GLP-1, the same hormone that GLP-1 receptor agonists mimic. By prolonging the action of GLP-1, DPP-4 inhibitors can improve insulin release and lower blood sugar levels. Compared to other diabetes medications, DPP-4 inhibitors tend to have a milder effect on blood sugar and are generally well-tolerated. I’ve heard many people say they appreciate the fact that they have a lower risk of hypoglycemia compared to sulfonylureas.
Thiazolidinediones (TZDs): Improving Insulin Sensitivity
Thiazolidinediones, or TZDs, are medications that improve your body’s sensitivity to insulin. They work by activating a receptor called PPARγ, which helps regulate glucose and lipid metabolism. TZDs can be effective at lowering blood sugar, but they can also cause side effects such as weight gain and fluid retention. They may not be suitable for people with heart failure or other cardiovascular conditions.
Insulin: The Original Solution
Insulin is a hormone that’s essential for regulating blood sugar levels. In type 1 diabetes, the body doesn’t produce insulin at all, while in type 2 diabetes, the body may not produce enough insulin or may become resistant to its effects. Insulin therapy involves injecting insulin to supplement or replace the body’s own insulin production. There are different types of insulin, including rapid-acting, short-acting, intermediate-acting, and long-acting insulin. The type of insulin and the dosage will depend on your individual needs and blood sugar levels.
Navigating Side Effects and Interactions
Like all medications, diabetes drugs can cause side effects. It’s important to be aware of the potential side effects of each medication and to discuss any concerns with your doctor. Some common side effects include nausea, diarrhea, hypoglycemia, weight gain, and skin rashes. It’s also important to be aware of potential drug interactions. Some medications can interact with diabetes drugs, affecting their effectiveness or increasing the risk of side effects. Always inform your doctor about all the medications you’re taking, including over-the-counter drugs and supplements.
Personalized Medicine: Finding the Right Fit for You
Diabetes management is not a one-size-fits-all approach. The best medication or combination of medications will depend on your individual needs, preferences, and health conditions. Factors such as age, weight, kidney function, and other medical conditions can all influence the choice of medication. Working closely with your doctor is essential to develop a personalized treatment plan that’s right for you. With the increasing prevalence of personalized medicine, your doctor will try to find something uniquely suitable for you.
| Medication Class | Mechanism of Action | Common Side Effects |
|---|---|---|
| Metformin | Decreases glucose production in the liver, improves insulin sensitivity | Gastrointestinal issues (nausea, diarrhea) |
| Sulfonylureas | Stimulates the pancreas to release more insulin | Hypoglycemia, weight gain |
| SGLT2 Inhibitors | Prevents the kidneys from reabsorbing glucose | Urinary tract infections, yeast infections, dehydration |
| GLP-1 Receptor Agonists | Mimics the effects of GLP-1, promoting insulin release and suppressing glucagon | Nausea, vomiting, diarrhea, weight loss |
| DPP-4 Inhibitors | Prevents the breakdown of GLP-1 | Generally well-tolerated, may cause mild side effects |
| Thiazolidinediones (TZDs) | Improves insulin sensitivity | Weight gain, fluid retention, heart failure |
| Insulin | Replaces or supplements the body’s own insulin production | Hypoglycemia, weight gain, injection site reactions |
Wrapping Up
Diving into the specifics of diabetes medications can feel overwhelming, but it’s a crucial step toward managing your health effectively. Remember, the best approach is a personalized one, tailored to your unique needs and lifestyle. Always work closely with your healthcare team to navigate these options and find the right fit for you. Don’t hesitate to ask questions and advocate for your well-being – you’re the expert on your own body, after all.
Handy Tips to Keep in Mind
1. Regular Blood Sugar Monitoring: Track your levels consistently to understand how different medications and lifestyle choices impact your health.
2. Balanced Diet is Key: Focus on whole foods, limit processed sugars, and plan meals to manage blood sugar spikes.
3. Stay Active: Incorporate regular physical activity into your routine to improve insulin sensitivity and overall health.
4. Hydration Matters: Drink plenty of water, especially if you’re taking medications that increase glucose excretion through urine.
5. Don’t Skip Doctor’s Appointments: Regular check-ups are essential for monitoring your health and adjusting your treatment plan as needed.
Key Takeaways
Understanding the different classes of diabetes medications is essential for effective diabetes management. Each class works uniquely to lower blood sugar levels, and knowing the basics empowers you to have more informed conversations with your doctor.
Metformin is often the first medication prescribed for type 2 diabetes. It primarily works by decreasing glucose production in the liver and improving your body’s sensitivity to insulin. Sulfonylureas and glinides stimulate your pancreas to release more insulin. SGLT2 inhibitors prevent the kidneys from reabsorbing glucose back into the blood, instead allowing excess glucose to be excreted in the urine. GLP-1 receptor agonists mimic the effects of a natural hormone called glucagon-like peptide-1 (GLP-1). DPP-4 inhibitors work by preventing the breakdown of GLP-1, the same hormone that GLP-1 receptor agonists mimic.
Thiazolidinediones, or TZDs, are medications that improve your body’s sensitivity to insulin. Insulin therapy involves injecting insulin to supplement or replace the body’s own insulin production.
Frequently Asked Questions (FAQ) 📖
Q: I just got diagnosed with type 2 diabetes. My doctor prescribed Metformin, but I’ve heard it can cause some pretty gnarly side effects. What are the most common side effects of Metformin, and is there anything I can do to minimize them?
A: Okay, so Metformin is like the OG drug for type 2 diabetes, but yeah, it can definitely have some unwelcome guests crashing the party in your gut. The most common side effects are nausea, diarrhea, and just a general feeling of “ugh” in your stomach.
I’ve seen people struggling with this a lot, especially when they first start taking it or if the dose is increased too quickly. Here’s the deal: always take it with food – that’s a biggie!
Also, ask your doctor about starting with a low dose and gradually increasing it. Sometimes, switching to the extended-release version can make a world of difference too.
And hey, if it’s really messing you up, don’t just grin and bear it; talk to your doctor. There are other options out there.
Q: My doctor mentioned something about SGLT2 inhibitors. What are they, and are they better than the older medications like sulfonylureas? I’m trying to avoid weight gain if I can, as that’s been an issue in the past.
A: SGLT2 inhibitors are the cool kids on the diabetes block these days. Think of them as sugar ninjas – they help your kidneys kick out extra glucose through your urine.
This not only lowers your blood sugar but can also lead to some weight loss, which is a huge win if you’re trying to avoid packing on pounds. Now, are they better than sulfonylureas?
That’s a tricky question because it really depends on your individual situation. Sulfonylureas are older, cheaper, and they work by squeezing more insulin out of your pancreas.
While effective, they can sometimes cause low blood sugar (hypoglycemia) and, unfortunately, weight gain. SGLT2 inhibitors, on the other hand, have a lower risk of hypoglycemia and can even offer some cardiovascular benefits.
However, they do come with their own set of potential side effects, like urinary tract infections and yeast infections. So, it’s a conversation you really need to have with your doctor to weigh the pros and cons.
Q: I’ve read a lot about GLP-1 receptor agonists, and they seem like a good option. How do they work, and are they usually given as a shot? I have a bit of a needle phobia, so that’s kind of a big deal for me.
A: Alright, let’s tackle the GLP-1s! These drugs are pretty slick – they mimic a natural hormone in your body called GLP-1, which helps to lower blood sugar by stimulating insulin release (but only when your blood sugar is high), slowing down digestion, and reducing appetite.
It’s like they’re multitasking your diabetes management. Now, to answer your question about the shot – yes, traditionally, most GLP-1s are administered as injections.
But (and this is a big “but”), there are now some oral GLP-1 receptor agonists available! So, definitely talk to your doctor about whether an oral option would be suitable for you.
As for the injections, they’re usually pretty painless and come in pens with very fine needles. Still, it’s understandable to be a little apprehensive.
If needles really freak you out, let your doctor know, and they can walk you through the process or explore alternatives. Don’t let a phobia prevent you from getting the best possible treatment.
📚 References
Wikipedia Encyclopedia
구글 검색 결과
구글 검색 결과
구글 검색 결과
구글 검색 결과
구글 검색 결과




